Estradiol (E2) is a medication and naturally occurring steroid hormone. It is an estrogen and is used mainly in menopausal hormone therapy and to treat low sex hormone levels in women. It is also used in hormonal birth control for women, in feminizing hormone therapy for transgender women, and in the treatment of hormone-sensitive cancers like prostate cancer in men and breast cancer in women, among other uses. Estradiol can be taken by mouth, held and dissolved under the tongue, as a gel or patch that is applied to the skin, in through the vagina, by injection into muscle or fat, or through the use of an implant that is placed into fat, among other routes.
Progynova (estradiol valerate) 2 mg oral tablets.
Generic estradiol (Mylan) 100 μg/day once-weekly transdermal patches.
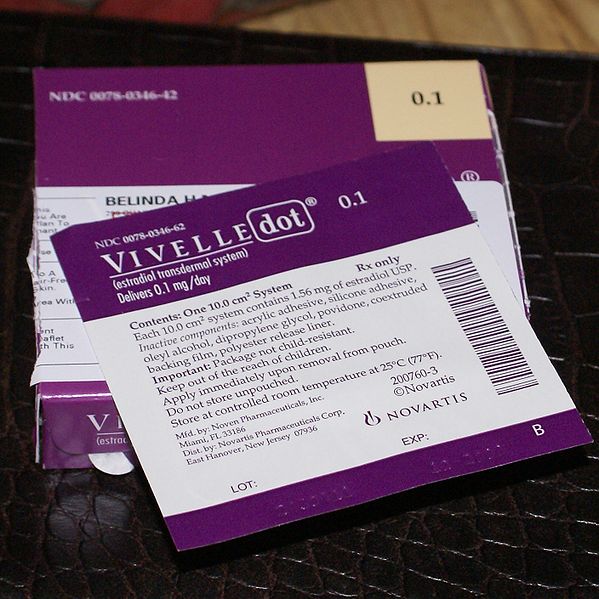
Vivelle-Dot (estradiol) 100 μg/day twice-weekly transdermal patches.
EstroGel 0.06% (estradiol) once-daily hydroalcoholic transdermal gel. Delivers 0.75 mg estradiol per pump.
Hormone replacement therapy
Hormone replacement therapy (HRT), also known as menopausal hormone therapy or postmenopausal hormone therapy, is a form of hormone therapy used to treat symptoms associated with female menopause. Effects of menopause can include symptoms such as hot flashes, accelerated skin aging, vaginal dryness, decreased muscle mass, and complications such as osteoporosis, sexual dysfunction, and vaginal atrophy. They are mostly caused by low levels of female sex hormones that occur during menopause.
Clot in the greater saphenous vein; oral estrogen is associated with increased risk of venous blood clots due to increased liver formation of vitamin K-dependent clotting factors.