The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate maternal and fetal circulations, and is an important endocrine organ, producing hormones that regulate both maternal and fetal physiology during pregnancy. The placenta connects to the fetus via the umbilical cord, and on the opposite aspect to the maternal uterus in a species-dependent manner. In humans, a thin layer of maternal decidual (endometrial) tissue comes away with the placenta when it is expelled from the uterus following birth. Placentas are a defining characteristic of placental mammals, but are also found in marsupials and some non-mammals with varying levels of development.
Human placenta from just after birth with the umbilical cord in place
Ultrasound image of human placenta and umbilical cord (color Doppler rendering) with central cord insertion and three umbilical vessels, at 20 weeks of pregnancy
Micrograph of a cytomegalovirus (CMV) infection of the placenta (CMV placentitis). The characteristic large nucleus of a CMV-infected cell is seen off-centre at the bottom-right of the image. H&E stain.
Human placenta immediately post birth.
In a multicellular organism, an organ is a collection of tissues joined in a structural unit to serve a common function. In the hierarchy of life, an organ lies between tissue and an organ system. Tissues are formed from same type cells to act together in a function. Tissues of different types combine to form an organ which has a specific function. The intestinal wall for example is formed by epithelial tissue and smooth muscle tissue. Two or more organs working together in the execution of a specific body function form an organ system, also called a biological system or body system.
The liver and gallbladder of a sheep
Relationship of major animal lineages with indication of how long ago these animals shared a common ancestor. On the left, important organs are shown, which allows us to determine how long ago these may have evolved.
Strobilus of Equisetum telmateia
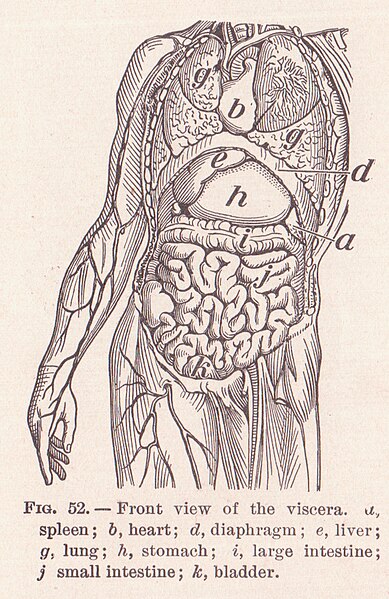
Human viscera